Trends in radiology and experimental research
Abstract
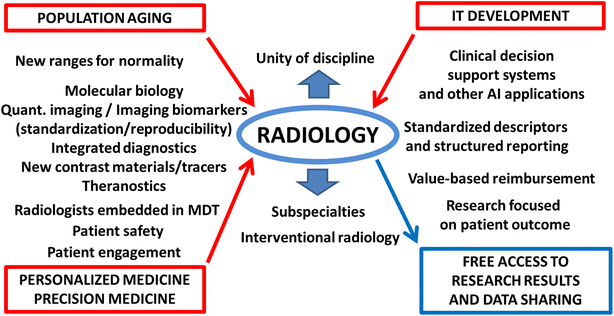
European Radiology Experimental, the new journal launched by the European Society of Radiology, is placed in the context of three general and seven radiology-specific trends. After describing the impact of population aging, personalized/precision medicine, and information technology development, the article considers the following trends: the tension between subspecialties and the unity of the discipline; attention to patient safety; the challenge of reproducibility for quantitative imaging; standardized and structured reporting; search for higher levels of evidence in radiology (from diagnostic performance to patient outcome); the increasing relevance of interventional radiology; and continuous technological evolution. The new journal will publish not only studies on phantoms, cells, or animal models but also those describing development steps of imaging biomarkers or those exploring secondary end-points of large clinical trials. Moreover, consideration will be given to studies regarding: computer modelling and computer aided detection and diagnosis; contrast materials, tracers, and theranostics; advanced image analysis; optical, molecular, hybrid and fusion imaging; radiomics and radiogenomics; three-dimensional printing, information technology, image reconstruction and post-processing, big data analysis, teleradiology, clinical decision support systems; radiobiology; radioprotection; and physics in radiology. The journal aims to establish a forum for basic science, computer and information technology, radiology, and other medical subspecialties.
Introduction
The decision of the European Society of Radiology (ESR) to launch European Radiology Experimental occurred in the context of relevant trends influencing the future of radiology. In changing times, to explore (to experiment) new ways, methods, and opportunities is important for spreading awareness of changes and guiding adaption. This article describes these trends and how experimental research in radiology (and this new journal) can play a role. “Today’s research is tomorrow’s practice” [1], and experimental research is a key factor for entering the future through the main gate.
General and specific trends influencing radiology and radiological research. MDT, multidisciplinary team; IT, information technology; AI, artificial intelligence
Three general trends
Population aging
The first general trend is population aging, a major factor especially in Europe, North America, and China but also, although at a slower pace, in the rest of the world. In 2002, the United Nations defined population aging as unprecedented, pervasive, enduring, and with profound implications for many facets of human life [2]. Baby boomers are now aged. From 2010 to 2040, the population over 65 is expected to increase from 16.1 to 25.2% in more developed regions, and from 5.8 to 12.4% in less developed regions including China. The population over 80 will increase from 4.3 to 8.6%, and from 0.9 to 2.5%, respectively. In 2050, in more developed regions, one out of ten inhabitants will be over 80 [3].
Population aging has two major consequences. On the one side, physicians should extend their knowledge about physiology of advanced elderly, changing their paradigms about normality. To distinguish between normal and abnormal will become more challenging. What is the normal range of cardiac ejection fraction or the normal glomerular filtration rate of a 90-year-old healthy subject? What about normal size of subarachnoid spaces in the advanced elderly? Indeed, we need studies to generate new reference ranges, which also consider the increasing ethnic diversity due to migration, especially in Europe.
On the other side, aging determines epidemiologic trends. Ischemic and hypertensive heart disease, stroke, pulmonary infections, cancer, and diabetes still remain the most relevant causes of death in middle-upper and high income countries, with dementia being a major problem for healthcare systems in high income countries [4]. Image-based innovations in risk stratification, screening, clinical diagnosis, interventional therapy, and prognosis in these fields will be welcomed by the journal. Although risk stratification, screening, and prognosis seem to be outside the area of experimental research, this is not true. Image-based techniques and methods need tests, refinements, and specifications before they may be used in practice, as explained below when considering quantitative radiology. This is also the key for acquiring a deeper knowledge of the physiology of advanced elderly.
Personalized and precision medicine
The second general trend includes personalized medicine, an approach which considers the individual characteristics of each subject for disease susceptibility, biology, and prognosis of diseases, and response to treatment. When the goal is to create a new taxonomy of human diseases based on molecular biology, we refer to the so-called precision medicine [5, 6]. This new patient-centred approach has profound implications for risk stratification and tailored screening or surveillance programs and personalized therapies. Molecular biology has a potential partnership with molecular imaging. As recently addressed by the ESR [7], imaging biomarkers can be used in all these steps, if our community is able to solve the challenge of standardization and reproducibility [8]. The relation between imaging features and genomics (radiogenomics) is adding more value to this patient-centred approach [9]. Biobanks and imaging biobanks will also play a role [10]. Potential exists for a future integrated diagnostics framework including both imaging and pathology, the latter of which has just become digital, as imaging is since many years.
Personalized and precision medicine does not end with the individual patient or patient’s disease. In oncology, tumour heterogeneity should be assumed as a major factor determining response to therapies [11]. A biopsy-based approach to multiple tumour lesions has practical limitations. Thus, radiology is well positioned for mapping cancer heterogeneity in the individual patient and guiding the adaptive therapy, especially if molecular imaging, radiomics, radiogenomics and habitat imaging techniques are used [6, 12, 13].
Patient engagement will improve personalized medicine, especially through the increasing use of mobile technology and the Internet. Automated emailing and interactive patient portals are already playing a role, offering the possibility of electronic access to medical records, images and reports [14]. Further research is expected on new software solutions for patient engagement in radiology, from scheduling procedures to follow-up examination reminders.
In the context of personalized and precision medicine, the research on contrast materials and tracers will play a big role. On the one hand, we should rethink individual dosages. One possibility is to consider the lean mass instead of the bodyweight for dose tailoring [15, 16, 17]. On the other hand, the development of new contrast materials and tracers will make the perspective for personalized and precision medicine more feasible. In this regard, theranostics, i.e. disease imaging and therapy together (targeted molecular imaging to follow the drug delivery pathway), is the most fascinating direction to follow [18].
Information technology development
Information technology (IT) development is one of the most important trends impacting individual and social life worldwide. From current applications on mobile phones and tablets to applications of artificial intelligence (AI) to medicine, our future will be strongly influenced by IT. Radiology was the leading discipline in the medical digital era [6]. Thus, relevant IT and AI innovations are expected in radiology and we should try to keep a prominent position as IT innovators in the arena of medical specialties. To this aim, the cooperation with IT scientists is necessary.
Advanced techniques of quantitative imaging, AI applications to clinical decision support systems, and big data analysis are only a few examples of radiology-specific trends coming from IT development.
Seven radiology-specific trends
Subspecialties versus unity of discipline
The tension between subspecialties and the unity of the discipline is increasing. Radiology subspecialties have a long history, with neuroradiology being one major paradigm of full dedication [19]. Interventional radiology inclined to claim for becoming “a primary specialty with uniquely trained clinicians” [20] or “an almost autonomous clinical specialty” [21]. To have radiologists subspecialized in specific fields is an obligatory way to answer clinical needs, to maintain our central role in multidisciplinary teams, and last but not least, to guide both experimental and clinical research. The radiologist embedded in a clinical team seems to be the best model of radiology consultation, with a non-negligible trade-off paid to productivity [22]. Are we risking a fragmentation of radiology?
To retain the unity of the discipline is not an old conservative academic viewpoint but a current need, as shown by the following considerations: 1. General previous training can be an advantage in comparison to clinicians who practice imaging in their field (“neuroradiologists may offer a differential diagnosis that includes non-neurologic conditions based on their more general training” [19]); 2. Modern imaging techniques commonly explore the body of the patient also outside the area of interest (in the case of cardiac computed tomography, the detection of a lung tumour can be more important than coronary stenosis quantification [23]); moreover, in multidisciplinary cancer teams, radiologists are frequently asked for their opinion about diagnosis and interventional treatments of metastases all over the body; 3. The distinction among subspecialties is blurred, important fields are cross-bordered, and the identity of subspecialties is always changing and evolving while imaging techniques migrate from one subspecialty to another; 4. Organizational aspects favour a central radiology department due to the impossibility to have radiologists dedicated exclusively to one subspecialty; additionally, a central radiology department able to manage large and expensive equipment allows a more cost-effective work-flow; 5. Some hybrid systems require the combination of radiology and nuclear medicine expertise, suggesting a unified training program as has already been initiated under the unique “Radiology” denomination in 2014 in The Netherlands [24].
Patient safety
A patient-centred approach also includes patient safety, in particular radioprotection, as highlighted by the European Society of Radiology (ESR) [25]. Radiologists should acknowledge the efforts made by the industry for a reduction of x-ray exposure, especially for computed tomography (CT). The possibility of performing coronary CT studies with much less than 1 mSv has been demonstrated [26, 27], while thoracic CT can be performed with less than 1 mSv (unenhanced studies) and less than 2 mSv (contrast-enhanced studies) [28].
These dramatic improvements imply two consequences. First, as suggested by the ESR [29], renewal of radiological equipment will be one of the most important factor driving the ionizing radiation exposure reduction in the next years. Second, reporting of radiation dose, if not already required by local regulations, will become a routine practice as indicated by the European Union Council Directive 2013/59 [30]. More preclinical (especially on phantoms) and clinical research is still expected on radioprotection. Research about the use of new hardware and software is welcomed by our journal. A similar reasoning applies for studies aimed at reducing the dose of both iodinated and gadolinium-based contrast materials, the latter especially after the so-called “brain deposition” issue [31].
Quantitative imaging
Imaging procedures will provide more and more output, not only images but also clinical data, numbers, indices, the core of the so-called quantitative imaging. Digital images are intrinsically data [32]. In certain cases, data can be more important than images. Examples are bone mineral densitometry and trabecular bone score through dual energy x-ray absorptiometry, where reproducibility defines the smallest detectable difference and the time to follow-up [33, 34, 35, 36, 37]. This is crucial for imaging biomarkers to be used for radiomics and radiogenomics, in particular for MRI-derived parameters. Radiologists are generally not ready for this, being mainly trained for qualitative reporting. For a long time, quantitation has been limited to the use of electronic calipers for size or to region-of-interest-based measurements of tissue electronic density through Hounsfield units in CT.
We should not forget the counterintuitive evolution of imaging methods for evaluating the response to therapy of solid tumours, from the two-dimensional criteria (the cross-product) proposed by the World Health Organization in 1981 [38] to the one-dimension Response Evaluation Criteria in Solid Tumours (RECIST) 1.0 in 2000 [39], as well as the RECIST 1.1 simplification, including positron emission tomography only in 2009 [40]. Notably, the main requirement for any new parameter to be accepted by the non-radiological clinical world is reproducibility. This explains why a diameter is more reproducible than a cross-product and the slow adoption of volume measurement [41].
Without reaching reliable standardization and reproducibility, new imaging-derived parameters are deemed to remain research topics only. A lot of experimental work is needed on the path to an imaging biomarker development and acceptance, proving the concept, the mechanism, the principle, the efficacy and effectiveness up to its use as surrogate end-point in clinical studies [42].
Standardized and structured reporting
Radiologic reporting is evolving towards standardized descriptors and diagnostic categories, in the context of structured reports. The Breast Imaging Reporting and Data Systems (BI-RADS), more than two decades after its first introduction in 1993 [43, 44], has been imitated in many other fields of diagnostic imaging [45, 46, 47, 48, 49] and the practice of radiology will follow this trend to facilitate the information transfer to patients and clinicians, including other radiologists.
Search for a higher level of evidence
We will be increasingly asked to demonstrate that radiology works in favour of patients, not only in terms of diagnostic performance but also at higher levels of the evidence-based medicine hierarchy, which implies impact on treatment, patient outcome, and societal effects [50]. This is now practically evident in the paradigm shift from a fee-for-service to a value-based model for reimbursement [51], in the context of a reduction or at least an end of expansion of healthcare expenditure [52]. Even though this trend mainly implies large clinical studies, innovation in study design to show efficacy and effectiveness of radiological procedures can be proposed through our journal.
Increasing relevance of interventional radiology
A major trend is surely the increasing penetrance of interventional radiology, which is a fundamental asset to improve the clinical profile of radiology [20, 21]. The role of minimally invasive image-guided therapies will expand in the next years, especially concerning interventional oncology. For the next generations it is of crucial importance that we continue to lead the way in device and method innovation in interventional radiology.
However, we should also try to build higher levels of evidence in favour of interventional radiology compared with standard methods, competing with other specialists working in the field [21]. Notably, the innovation of devices and methods is an easier task than building high-level evidence, as “most interventional radiologists lack expertise in the relatively challenging advanced methods used in comparative effectiveness and cost-effectiveness research” [20]. This challenge implies efforts in education and mentoring, beginning with training during post-graduation schools.
Technological evolution
Last but not least, we have to consider the continuous technological evolution of existing imaging methods, the introduction of new imaging methods as well as various effects of IT and AI development in the field of medical imaging.
The general economic context will probably favour the evolution of existing imaging methods more than the introduction of new imaging methods. Imaging procedures will become faster and faster, as has already happened with CT and MRI, while new hybrid technologies will be proposed. An intriguing evolution of existing methods could be an unprecedented portability of imaging devices [6], especially in the emergency setting [53]. While phase-contrast x-ray may bring relevant innovations to radiodiagnostics [54, 55, 56], optical and photo-acoustic imaging may come to clinical practice [57, 58].
We should also take into consideration a sceptical view, such as that proposed by Eugen Lin in 2011, when he wrote [52]: “In many cases, our technology has reached a point where the marginal value of further advances for patient care may be minimal. […] I believe that there will be substantially fewer technologic advances implemented in routine clinical practice in the near future. But what of the much-touted molecular imaging? Although I do not doubt the potential of molecular imaging compared with existing anatomic imaging techniques, molecular imaging techniques will likely face the same substantial hurdles to reimbursement”. In any case, the initial evidence provided for new modalities or techniques in the experimental setting will be necessary for translation into clinical practice. European Radiology Experimental will provide a forum for this.
Among the technological evolution we can include IT development. Radiology information systems will be integrated in hospital and regional/national health information systems. All areas of innovation in this field and their interplays require research by radiologists and IT experts, as outlined by Nance et al. [59]: aggregation of electronic medical records, allowing radiologists to access clinical information (not only information provided by ordering clinicians) at hand when defining the protocol of a procedure or interpreting images, immediate use of clinical decision support systems for ordering, interpreting, and defining further patient management, internal peer review, tracking of resident training, communication of critical findings, quality control of technologists’ performances and communication between radiologists and technologists, customer service towards patients and referring physicians, surveillance and outcome measures, and data mining regarding previous issues (including radiation dose).
It is easy to predict that AI will be increasingly implemented in medical imaging systems. Examples of this trend are computer aided detection and diagnosis, advanced image analysis, such as texture energy and deep learningmethods [6], fusion imaging, three-dimensional printing, structured reporting and new models of relations of radiologists with patients and referring physicians, teleradiology.
In particular, clinical decision support systems will be used by radiologists (management of additional findings, ordering additional imaging or biopsy, image interpretation) and other clinicians (importantly, when ordering imaging studies). As a general effect, these systems should result in an increase in the meaningful and appropriate use of radiology [60]. The available knowledge on medicine and medical imaging is superior to any human ability to memorize and correctly exploit it in favour of patients. Even considering imaging-related articles only, hundreds of new reports appear online daily. When searching PubMed for papers including “imaging” or “radiology”, the number of items obtained per year is 42,757 in 2000, 60,956 in 2005, 94,623 in 2010, 130,353 in 2015; from 2000 to 2015 the number of items per day went up from 117 to 357, more than a three-fold increase [61]. Only the smart use of information technology can allow us for taking advantage of this amount of available information.
Nowadays, when typical randomized controlled trials or large prospective comparative studies imply high costs, proper analysis of the big data we already have in our radiology information systems [62] can allow for transforming stored information into new knowledge. In the hierarchy of understanding, an increasing organizational level grows from data (discrete elements) to information (linked elements), to knowledge (organized information), and to wisdom (applied knowledge) [63]. Studies on radiological data in this direction are welcome.
Experimental research in radiology and the structure of the journal
Radiologists will have to contribute to and guide future research projects regarding the above described trends. It is not only a matter of innovation in devices and products, but also a matter of innovation of processes and methods. Testing devices, products and methods in an experimental setting is always the first step.
Notably, the word experimental has a wide spectrum of meanings, providing many opportunities for this journal. Most commonly regarded as experimental are imaging studies on phantoms, cells, or animal models. However, we also consider studies in which the observer properly modifies a given practice for a defined outcome to be measured (a planned variation under controlled conditions [64]) as “experimental”. Of course, this applies also to studies on humans and especially on explorative studies, such as those reporting secondary end-points of large clinical trials, studies which will also be considered for publication by the journal.
This profile implies a special characteristic of European Radiology Experimental: we need a strict cooperation between clinical imaging specialists (radiologists and nuclear physicians) and a large variety of other professionals involved in medical imaging development and application: biologists, chemists, bioengineers and biomathematicians, experts in computer science, information technology and bioinformatics, as well as other physicians working in medical imaging such as pathologists, geneticists, neurologists, surgeons, cardiologists, and many more. The journal will establish a public forum for this large community.
-
Biomathematics and computer modelling
-
Contrast materials, tracers, and theranostics
-
Experimental models of human disease
-
Information technology, big data, image reconstruction and post-processing
-
Imaging biomarkers, radiomics, radiogenomics, and imaging biobanks
-
Interventional
-
Metabolic and functional imaging
-
Methodology and statistics
-
Molecular and hybrid imaging
-
Novel imaging modalities/techniques
-
Radiobiology, radioprotection, and physics in radiology
As per the aims and scope of the journal, about 50% of the Editorial Board members are neither radiologists nor nuclear physicians, thus including expertise from many other fields. I thank all board members for taking part in this initiative.
Conclusions
Considering the above described trends, European Radiology Experimental joins the ESR journal family as an online only and fully (gold) open access journal. This follows the guidelines defined by the European Union: papers deriving from projects supported by public funds should be freely available for reading by 2020 [65]. The discussion about free access to data supporting the results of scientific research (the so-called data sharing [66]) is ongoing and this accessibility should be combined also with ethical, economic, and authorship issues. European Radiology Experimental encourages data sharing and will work in favour of this.
“The future cannot be predicted, but futures can be invented”, said Dennis Gabor, the Hungarian Engineer who received the 1971 Nobel Prize in Physics for the invention of holography [67]. Of course, this cannot be achieved through journals alone, but the ESR is already driving relevant processes, working for the next generation of radiologists. In these changing times, European Radiology Experimental can play a pivotal role.
Declarations
Acknowledgements
Thanks to Regina Beets-Tan, Giovanni Di Leo, Gabriel Krestin, Maximilian Reiser, and Luca Maria Sconfienza for reading different versions of the article and giving remarkable suggestions.
Competing interests
The author declares that he has no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Authors’ Affiliations
References
- Dunnick NR (2003) Report of the 2002 Intersociety Commission meeting: Radiology 2002—today’s research is tomorrow’s practice. AJR Am J Roentgenol 180:925–928View ArticlePubMedGoogle Scholar
- United Nations. Department of Economic and Social Affairs, Population Division. World Population Ageing: 1950-2050. Available at: http://www.un.org/esa/population/publications/worldageing19502050/. Accessed on 1 Jan 2017
- United Nations, Department of Economic and Social Affairs, Population Division (2015) World Population Prospects: The 2015 Revision, custom data acquired via website. Available at: https://esa.un.org/unpd/wpp/DataQuery/. Accessed on 1 Jan 2017
- World Health Organization (2012) The 10 leading causes of death by country income group. Available at: http://www.who.int/mediacentre/factsheets/fs310/en/index1.html. Accessed on 1 Jan 2017
- United States National Research Council (2011) National Research Council of the National Academies white paper: toward precision medicine: building a knowledge network for biomedical research and a new taxonomy of disease. The National Academies Press, WashingtonGoogle Scholar
- Thrall JH (2016) Trends and developments shaping the future of diagnostic medical imaging: 2015 Annual oration in diagnostic radiology. Radiology 279:660–666View ArticlePubMedGoogle Scholar
- European Society of Radiology (2015) Medical imaging in personalised medicine: a white paper of the research committee of the European Society of Radiology (ESR). Insights Imaging 6:141–155View ArticleGoogle Scholar
- European Society of Radiology (2013) ESR statement on the stepwise development of imaging biomarkers. Insights Imaging 4:147–152View ArticleGoogle Scholar
- Rutman AM, Kuo MD (2009) Radiogenomics: creating a link between molecular diagnostics and diagnostic imaging. Eur J Radiol 70:232–241View ArticlePubMedGoogle Scholar
- European Society of Radiology (2015) ESR Position Paper on Imaging Biobanks. Insights Imaging 6:403–410Google Scholar
- Welch DR (2016) Tumor Heterogeneity—A ‘contemporary concept’ founded on historical insights and predictions. Cancer Res 76:4–6View ArticlePubMedPubMed CentralGoogle Scholar
- Kumar V, Gu Y, Basu S et al (2012) Radiomics: the process and the challenges. Magn Reson Imaging 30:1234–1248View ArticlePubMedPubMed CentralGoogle Scholar
- Sala E, Mema E, Himoto Y et al (2017) Unravelling tumour heterogeneity using next-generation imaging: radiomics, radiogenomics, and habitat imaging. Clin Radiol 72:3–10View ArticlePubMedGoogle Scholar
- Morgan TA, Avrin DE, Carr CD et al (2013) Meaningful use for radiology: current status and future directions. Radiology 269:318–321, Erratum in Radiology 2014;270:314View ArticlePubMedGoogle Scholar
- Kondo H, Kanematsu M, Goshima S et al (2013) Body size indices to determine iodine mass with contrast-enhanced multi-detector computed tomography of the upper abdomen: does body surface area outperform total body weight or lean body weight? Eur Radiol 23:1855–1861View ArticlePubMedGoogle Scholar
- Awai K, Kanematsu M, Kim T, Ichikawa T et al (2016) The optimal body size index with which to determine iodine dose for hepatic dynamic CT: A prospective multicenter study. Radiology 278:773–781View ArticlePubMedGoogle Scholar
- Zanardo M, Doniselli FM, Esseridou A, Tritella S, Di Leo G, Sardanelli F. (2017) Contrast dose variability depending on morphometric values: a retrospective analysis on patients undergoing multi-phase abdominal CT. Insight Imaging (Oral presentation at ECR 2017 -Number: 5015)Google Scholar
- Terreno E, Uggeri F, Aime S (2012) Image guided therapy: the advent of theranostic agents. J Control Release 161:328–337.Google Scholar
- Bello J (2012) Turf issues in radiology and its subspecialties. Neuroimaging Clin N Am 22:411–419View ArticlePubMedGoogle Scholar
- Kwan SW, Talenfeld AD, Brunner MC (2016) The top three health care developments impacting the practice of interventional radiology in the next decade. AJR Am J Roentgenol 207:731–736.View ArticleGoogle Scholar
- Makris GC, Uberoi R (2016) Interventional radiology- The future: Evolution or extinction? Cardiovasc Intervent Radiol 39:1789–1790Google Scholar
- Gunderman RB, Chou HY (2016) The future of radiology consultation. Radiology 281:6–9View ArticlePubMedGoogle Scholar
- Flor N, Di Leo G, Squarza SA et al (2013) Malignant incidental extracardiac findings on cardiac CT: systematic review and meta-analysis. AJR Am J Roentgenol 201:555–564View ArticlePubMedGoogle Scholar
- Holscher HC (2016) Hybrid imaging: the Dutch approach. Presentation at the ESR Leadership Meeting. Barcelona, 17 Nov 2016Google Scholar
- European Society of Radiology (ESR) Eurosafe Imaging. Available at: http://www.eurosafeimaging.org/. Accessed on 4 Jan 2017
- Achenbach S, Marwan M, Ropers D et al (2010) Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J 31:340–346View ArticlePubMedGoogle Scholar
- Schuhbaeck A, Achenbach S, Layritz C et al (2013) Image quality of ultra-low radiation exposure coronary CT angiography with an effective dose <0.1 mSv using high-pitch spiral acquisition and raw data-based iterative reconstruction. Eur Radiol 23:597–606View ArticlePubMedGoogle Scholar
- den Harder AM, Willemink MJ, de Ruiter QM et al (2015) Achievable dose reduction using iterative reconstruction for chest computed tomography: A systematic review. Eur J Radiol 84:2307–2313View ArticleGoogle Scholar
- European Society of Radiology (2014) Renewal of radiological equipment. Insights Imaging 5:543–546View ArticleGoogle Scholar
- European Union (2013) Council Directive 2013/59/Euratom, 5 December 2013. Available at: https://ec.europa.eu/energy/sites/ener/files/documents/CELEX-32013L0059-EN-TXT.pdf. Accessed on 4 Jan 2017
- Malayeri AA, Brooks KM, Bryant LH et al (2016) National Institutes of Health perspective on reports of Gadolinium deposition in the brain. J Am Coll Radiol 13:237–241View ArticlePubMedPubMed CentralGoogle Scholar
- Gillies RJ, Kinahan PE, Hricak H (2016) Radiomics: Images are more than pictures, they are data. Radiology 278:563–577View ArticlePubMedGoogle Scholar
- Delnevo A, Bandirali M, Di Leo G et al (2013) Differences among array, fast array, and high-definition scan modes in bone mineral density measurement at dual-energy x-ray absorptiometry on a phantom. Clin Radiol 68:616–619View ArticlePubMedGoogle Scholar
- Bandirali M, Sconfienza LM, Aliprandi A et al (2014) In vivo differences among scan modes in bone mineral density measurement at dual-energy X-ray absorptiometry. Radiol Med 119:257–260View ArticlePubMedGoogle Scholar
- Bandirali M, Poloni A, Sconfienza LM et al (2015) Short-term precision assessment of trabecular bone score and bone mineral density using dual-energy X-ray absorptiometry with different scan modes: an in vivo study. Eur Radiol 25:2194–2198View ArticlePubMedGoogle Scholar
- Bandirali M, Di Leo G, Messina C et al (2015) Reproducibility of trabecular bone score with different scan modes using dual-energy X-ray absorptiometry: a phantom study. Skeletal Radiol 44:573–576View ArticlePubMedGoogle Scholar
- Messina C, Bandirali M, Sconfienza LM et al (2015) Prevalence and type of errors in dual-energy x-ray absorptiometry. Eur Radiol 25:1504–1511View ArticlePubMedGoogle Scholar
- Miller AB, Hoogstraten B, Staquet M, Winkler A (1981) Reporting results of cancer treatment. Cancer 47:207–214View ArticlePubMedGoogle Scholar
- Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216Google Scholar
- Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247View ArticlePubMedGoogle Scholar
- Sardanelli F, Esseridou A, Del Sole A, Sconfienza LM (2012) Response to treatment: the role of imaging. In: Aglietta M, Regge D (eds) Imaging tumor response to therapy. Springer, Milan, pp 15–36View ArticleGoogle Scholar
- Martí Bonmatí L, Alberich-Bayarri A, García-Martí G et al (2012) Imaging biomarkers, quantitative imaging, and bioengineering. Radiologia 54:269–278View ArticlePubMedGoogle Scholar
- American College of Radiology (1993) Breast Imaging Reporting and Data System (BI-RADS), 1st edn. American College of Radiology, RestonGoogle Scholar
- Burnside ES, Sickles EA, Bassett LW et al (2009) The ACR BI-RADS experience: learning from history. J Am Coll Radiol 6:851–860View ArticlePubMedPubMed CentralGoogle Scholar
- Barentsz JO, Richenberg J, Clements R (2012) ESUR prostate MR guidelines. Eur Radiol 22:746–757View ArticlePubMedPubMed CentralGoogle Scholar
- Cheng SP, Lee JJ, Lin JL et al (2013) Characterization of thyroid nodules using the proposed thyroid imaging reporting and data system (TI-RADS). Head Neck 35:541–547View ArticlePubMedGoogle Scholar
- Manos D, Seely JM, Taylor J et al (2014) The Lung Reporting and Data System (LU-RADS): a proposal for computed tomography screening. Can Assoc Radiol J 65:121–134Google Scholar
- Pooler BD, Kim DH, Lam VP et al (2014) CT Colonography Reporting and Data System (C-RADS): benchmark values from a clinical screening program. AJR Am J Roentgenol 202:1232–1237Google Scholar
- Mitchell DG, Bruix J, Sherman M et al (2015) LI-RADS (Liver Imaging Reporting and Data System): Summary, discussion, consensus of the LI-RADS Management Working Group and future directions. Hepatology 61:1056–1065View ArticlePubMedGoogle Scholar
- Sardanelli F, Hunink MG, Gilbert FJ, Di Leo G, Krestin GP (2010) Evidence-based radiology: why and how? Eur Radiol 20:1–15View ArticlePubMedGoogle Scholar
- Sarwar A, Boland G, Monks A, Kruskal JB (2015) Metrics for radiologists in the era of value-based health care delivery. Radiographics 35:866–876View ArticlePubMedGoogle Scholar
- Lin E (2011) Radiology 2011: the big picture. AJR Am J Roentgenol 196:136–139View ArticlePubMedGoogle Scholar
- O’Connell TW, Patlas MN (2016) Mobile devices and their prospective future role in emergency radiology. Br J Radiol 89:20150820View ArticlePubMedPubMed CentralGoogle Scholar
- Bravin A, Coan P, Suortti P (2013) X-ray phase-contrast imaging: from pre-clinical applications towards clinics. Phys Med Biol 58:R1–35View ArticlePubMedGoogle Scholar
- Auweter SD, Herzen J, Willner M et al (2014) X-ray phase-contrast imaging of the breast—advances towards clinical implementation. Br J Radiol 87:20130606View ArticlePubMedPubMed CentralGoogle Scholar
- Hetterich H, Willner M, Habbel C et al (2015) X-ray phase-contrast computed tomography of human coronary arteries. Invest Radiol 50:686–694View ArticlePubMedGoogle Scholar
- Dong B, Sun C, Zhang HF (2017) Optical Detection of Ultrasound in Photoacoustic Imaging. IEEE Trans Biomed Eng 64:4–15View ArticlePubMedGoogle Scholar
- Grosenick D, Rinneberg H, Cubeddu R, Taroni P (2016) Review of optical breast imaging and spectroscopy. J Biomed Opt 21:091311View ArticlePubMedGoogle Scholar
- Nance JW Jr, Meenan C, Nagy PG (2013) The future of the radiology information system. AJR Am J Roentgenol 200:1064–1670View ArticlePubMedGoogle Scholar
- Morgan TA, Avrin DE, Carr CD et al (2013) Meaningful use for radiology: current status and future directions. Radiology 269:318–321View ArticlePubMedGoogle Scholar
- United States National Library of Medicine. National Institutes of Health. https://www.ncbi.nlm.nih.gov/pubmed. Data extracted on 3 Jan 2017
- Kansagra AP, Yu JP, Chatterjee AR et al (2016) Big data and the future of radiology informatics. Acad Radiol 23:30–42View ArticlePubMedGoogle Scholar
- McCandless D (2010) Data, Information, Knowledge, Wisdom?. 2010. Available at: http://www.informationisbeautiful.net/2010/data-information-knowledge-wisdom/. Accessed on 3 Jan 2017
- Sardanelli F, Di Leo G (2009) Biostatistics for Radiologists. Springer, Milan, pp 144–148View ArticleGoogle Scholar
- Khomami N (2016) All scientific papers to be free by 2020 under EU proposals. The Guardian, May 28, 2016. Available at: https://www.theguardian.com/science/2016/may/28/eu-ministers-2020-target-free-access-scientific-papers. Accessed on Jan 5, 2017
- Bauchner H, Golub RM, Fontanarosa PB (2016) Data sharing: an ethical and scientific imperative. JAMA 315:1237–1239PubMedGoogle Scholar
- World Press. Quote Investigator. Exploring the origins of quotations. Available at: http://quoteinvestigator.com/2012/09/27/invent-the-future/. Accessed on 3 Jan 2017